How to Make Your Own Stem Cells
There Are Now Multiple Ways Adult Stem Cells Can Be Turned Embryonic
There are many reasons a patient may need a tissue or blood transplant from a donor, and in many cases the problem of immune rejection is a major obstacle to be overcome. Consequently, researchers have increasingly focused on developing ways to heal damaged or diseased tissues by using a patient’s own cells.
There are now multiple types of stem cells that hold great promise for creating patient-specific cells for therapies.
Rejection of a transplant from a donor occurs when a patient’s immune system rejects the transplant tissue as foreign. It’s a normal (and usually healthy) process. The body is simply trying to protect itself from a foreign “invader,” just as it usually fights off viral and bacterial infection. Immune rejection is a common problem, depending on the kind of transplant being performed, and often long-term courses of immunosuppressant drugs are required over the patient’s lifetime to prevent rejection of the transplant.
But by using a patient’s own cells to repair the tissue, there should be no immune response triggered. At this point in time, two types of stem cells hold great promise for use in regenerative medicine where immune rejection is a significant concern: human induced pluripotent stem cells (iPSCs) and cells made through a process called somatic cell nuclear transfer (SCNT).
Both of these types of cells have the ability to become any type of cell in the body, and both can multiply virtually indefinitely.
These two characteristics are what give such promise to human embryonic stem cells (ESCs) (which very recently started to be used in clinical trials for treating spinal cord injuries). But unlike embryonic stem cells, iPSCs and cells from SCNT can be made using a patient’s own cells, making them patient-specific and avoiding immune rejection complications. Because iPSCs were focused on in a previous article, this one will focus on advances in SCNT technology and its therapeutic potential.
Somatic cell nuclear transfer (SCNT): SCNT technology significantly predates iPSCs, and, as was discussed previously, in many ways formed the basis for the idea of iPSCs. In SCNT, the nucleus (which holds the cell’s DNA) is taken from a matured, adult cell (all such cells are called “somatic” cells). This nucleus is implanted into an egg, which already had its own nucleus removed. Amazingly, the egg “reprograms” the nucleus to an embryonic state, together creating a new embryo but with the adult cell’s genetic lineage. It’s been found that SCNT causes some 10,000 to 12,000 genes to be activated that are normally only active during embryonic development. The newly formed embryo (technically called a blastocyst) can then be implanted into a surrogate mother, and potentially become an adult organism. This organism is a clone of the animal that donated the nucleus; they have identical DNA.
Although nuclear transfer studies have been conducted since the late 1930s, it wasn’t until 1997 that the first widely-accepted-as-successful use of SCNT was reported: Dolly the sheep was born, the first cloned animal from an adult cell. Since Dolly, several other animals have been successfully cloned, though many problems still remain. (Only about zero to 10 percent of embryos created through SCNT result in live births.)
Therapeutic cloning: While SCNT has been long-explored for its ability to create cloned animals like Dolly and others (a practice called “reproductive cloning”), SCNT has other very appealing applications that do not involve the creation of an entire animal—primarily “therapeutic cloning.” The goal of therapeutic cloning is to use SCNT technology to create patient-specific embryonic stem cells for medical therapies, such as regenerative medicine.
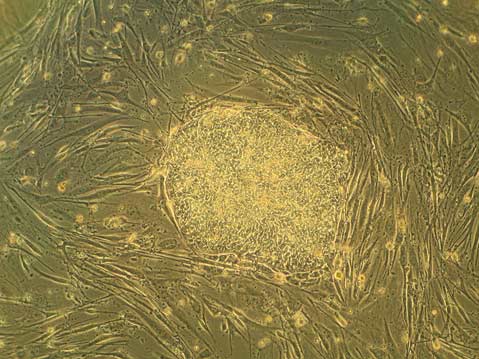
How can SCNT be used to create embryonic stem cells (ESCs)? Normally, ESCs are harvested from an embryo at the blastocyst stage. That’s when the embryo is four or five days post-fertilization and is a fluid-filled sphere containing approximately 150 cells. As was described above, SCNT creates embryos that are clones of the DNA donor. When a cloned embryo is at the blastocyst stage, ESCs can be harvested just as they are from a non-cloned blastocyst.
While using SCNT to clone an entire animal has been fraught with challenges, using SCNT to create ESCs for therapies may be less difficult since it only requires the formation of a very early-stage embryo.
SCNT-derived ESCs have been created from multiple types of animals.
SCNT and the mouse: In 2000, the first ESCs were made from mice using SCNT. These SCNT-derived mouse ESCs behaved similarly to, and had the same abilities as, normally-derived mouse ESCs. Not only could ESCs be successfully derived in this way, but studies in mice have also shown that SCNT can be used to repair genetic diseases, such as Parkinson’s or deficient immune systems.
Generally what is done in these studies is this: A mouse with a genetic defect undergoes SCNT. That is, it has the nucleus from one of its adult cells removed and placed into an enucleated mouse egg cell, ultimately creating ESCs. In these ESCs, the defect can be fixed using standard genetic techniques, and the repaired cells (after they have been made into the proper cell type) are transplanted back into the original donor mouse. Mice have been successfully cured of genetic diseases this way.
SCNT in non-human primates: In 2007, ESCs were created from a rhesus macaque, an Old World monkey, using SCNT. To accomplish this, Shoukhrat Mitalipov and colleagues at Oregon National Primate Research Center took the nucleus from a skin cell of a female rhesus macaque and had the nucleus undergo SCNT in the eggs of another female macaque. Although these ESCs looked and acted like normal ESCs, the process was far from perfect; the researchers had to use 304 eggs to make two lines of ESCs (this means they successfully isolated ESCs from two different blastocysts).
However, progress was quickly made and two years later Mitalipov’s group reported a three-fold increase in ESC generation from rhesus macaques using improved SCNT techniques. These levels are similar to those seen with the generation of ESC lines from normally fertilized embryos, giving researchers hope for transitioning the technology to humans.
Humans and SCNT: Currently, a scarcity of high-quality donated human eggs is the largest hurdle to creating patient-specific human ESCs through SCNT. There are also many technical issues that need to be optimized. But one of the greatest challenges is not technical, but social: In 2004, Woo Suk Hwang and colleagues in South Korea reported having created human ESCs through SCNT for the first time, but their work was proven to be fraudulent. Because of these falsified studies, subsequent researchers have had to go to great lengths to show that their SCNT data is valid, making it an even more difficult field in which to achieve progress.
Because of the lack of donated human eggs, researchers have pursued studies using eggs donated from other animals for SCNT. This technique is called human-animal interspecies SCNT (iSCNT). Many ethical concerns have been raised over the use of this technique, especially since an iSCNT embryo contains a human nucleus but also some other animal DNA (from the mitochondria). Additionally, some reports have suggested that iSCNT embryos are not “healthy,” primarily because the nucleus doesn’t completely return to an embryonic state. In one such study, a group of researchers combined the nucleus of an adult chimpanzee cell with an egg from a cow, but the embryos did not grow past having only 16 cells. It turned out that many genes that are essential for early development weren’t actually active.
There have also been reports of iSCNT being performed using human and animal cells, such as with a human nucleus and a rabbit egg. Overall, there are still many ethical and biological concerns surrounding the practice of iSCNT.
Despite the lack of available, donated human eggs and the lingering pall on the field from the fraudulent work of Hwang and colleagues, in 2008 several stem cell-oriented companies (including Stemagen Corporation and The Reproductive Sciences Center, both located in Southern California) collaboratively published the successful creation of human blastocysts from SCNT. In this study, 21 human eggs were donated with informed consent and each was combined with a nucleus from an adult skin cell through SCNT. From these 21 eggs and nuclei, five blastocysts were created, and at least one was proven to be a true clone of the donor.
The future: Although much work remains to be done before SCNT is a viable strategy for the production of patient-specific ESCs for regenerative medicine, there is enormous potential that such “therapeutic cloning” could fulfill when the technology matures. Not only may a patient have cells made that are specific to them and available as virtually any cell type they should need (such as insulin-producing beta cells for a patient with diabetes), but, for example, if they have a genetic disease this too may be cured (as was demonstrated in mice using this technology).
Researchers could also create cell lines from patients to study specific diseases in the laboratory, greatly advancing our understanding of these conditions ( this is currently being explored with iPSCs as well).
Lastly, as our ability to create ESCs from embryos improves in general, it should become easier to create SCNT-derived ESCs. As SCNT research has come close to being completely illegal in the United States, it’s important not only for researchers to always take proper ethical precautions, but for everyone to be aware of the great potential this technology holds, and to understand the big difference between “reproductive cloning” and “therapeutic cloning.”
Aside from stem cells derived from SCNT, a great variety of other stem cell types and technologies exist that hold much promise in the field of regenerative medicine. In particular: the very closely-related induced pluripotent stem cells; human embryonic stem cells , which very recently started to be used in clinical trials for treating spinal cord injuries; an assortment of adult stem cells; and a recently developed technique called “direct reprogramming.”
For more on the use of somatic cell nuclear transfer, see Teisha Rowland’s All Things Stem Cell post “Creating Patient-Specific Stem Cells Through Somatic Cell Nuclear Transfer”, Congresswoman Diana DeGette’s book Sex, Science, and Stem Cells, for the politics behind these issues, or Wikipedia’s article on Somatic cell nuclear transfer.
Biology Bytes author Teisha Rowland is a science writer, blogger at All Things Stem Cell, and graduate student in molecular, cellular, and developmental biology at UCSB, where she studies stem cells. Send any ideas for future columns to her at science@independent.com.



