Insurance Denied When Most Needed
Healing a Broken Health-Care System by Holding Insurers Accountable
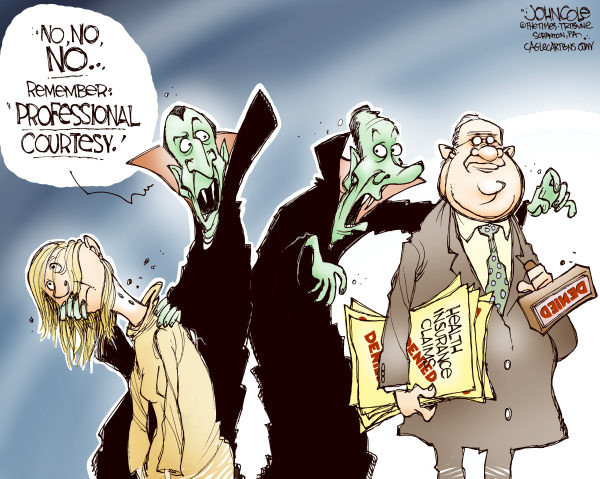
Recently, the state Supreme Court affirmed a $91 million fine against UnitedHealthcare, scoring a major victory for California patients who were wrongfully denied access to care by the insurance giant. The scale of violations by the insurer — topping more than 900,000 improper denials — demonstrates the power imbalance between patients and insurers.
While I was not one of the 900,000 denials, I learned firsthand how daunting a fight with an insurer can be when I was diagnosed with breast cancer at age 21. I assumed my health-care insurer would approve my physician-recommended care. I was wrong. Now, I’m joining others and calling on Congress to hold insurers accountable for providing cancer patients access to the treatments they need.
My experience ended well, but my journey shows what’s wrong with a system where broken insurance processes make it nearly impossible for cancer patients to receive the best care. While cancer interrupted my senior year of college at UC Santa Barbara, my insurer’s actions caused me the most stress. I eyed treatment bills for thousands of dollars and was terrified of the financial burden this could put on my family.
At the heart of my insurance fight was proton beam therapy. My doctors ruled out traditional radiation treatment as too risky because of a genetic susceptibility to secondary cancers. Proton therapy’s precision would target my tumor and minimize radiation exposure to healthy tissue, significantly reducing my risk of secondary cancer. It was a no-brainer to everyone but UnitedHealthcare.
My initial proton therapy request was met with a denial letter that cited outdated clinical guidelines from 2012 and called the treatment unproven and unnecessary. However, the guidelines had long been updated to recommend proton therapy for breast cancer patients.
My doctors appealed the decision but received another denial, this time with an opinion from a gynecologist with no knowledge of proton therapy. This unqualified reviewer determined that “other types of radiation would be equally effective,” ignoring the risk of secondary cancer that could shorten my life.
Thankfully, California Protons did not delay my treatment while I took my denial fight to the California insurance commissioner. Six months after I completed treatment, the commissioner overruled UnitedHealthcare and sided with my doctors. A financial burden was lifted.
Like me, many cancer patients are left waiting as insurers drag them through appeals and their cancers grow. In fact, a report from the Alliance for Proton Therapy Access found that four in ten cancer patients are initially denied care that their doctors recommend and wait more than five weeks on average before receiving a final denial. As any cancer survivor will tell you, we don’t have the luxury of time or the energy to play insurers’ games.
Just last year, UnitedHealthcare made national news after a series of denials forced one cancer survivor to rely on her parents’ retirement savings to cover her life-saving proton therapy. Another insurer’s broken processes landed it in an Oklahoma court, where a jury found the insurer guilty of reckless disregard after a rubber-stamp denial.
It’s time for federal legislators to examine this problem and stop improper denials. I’m joining advocates across the country in calling on lawmakers to adopt principles of a Cancer Patients’ Timely Treatment Bill of Rights into legislation.
I recently interned on Capitol Hill with my member of Congress and witnessed the power of grassroots advocacy. Now, it’s my turn to take action. I hope those impacted by cancer — survivors, patients, family members, and friends — will join me. Holding insurers accountable for treating cancer patients fairly is an issue all policymakers should support.
Mariam Tariq is a cancer survivor, an advocate with the Alliance for Proton Therapy Access, and UC Santa Barbra graduate.



