Can Santa Barbara County Hospitals Handle the Surge in COVID Patients?
Cottage’s Dr. Fitzgibbons Explains How ER Doctors Determine Who Is Admitted and Who Is Sent Home

With hospitals in many parts of the state and the country now bursting with COVID patients, the $64-million question has become: who is admitted and who is not? Who gets hospitalized and who is still well enough to get sent home? In Santa Barbara County, we haven’t got there yet, but the question is beginning to push the comfort level of infectious-disease specialists — such as Cottage Hospital’s Dr. Lynn Fitzgibbons — as the number of Santa Barbara’s County’s COVID patients requiring hospital beds has jumped significantly since this June.
Most people who get infected are never hospitalized. Since March, 4,323 county residents have tested positive for COVID-19. Of those, 3,921 have recovered.
As of this writing on July 14, Santa Barbara County has 371 active COVID cases. For us, that’s on the high side, but it has declined since the 444 patients recorded couple weeks ago. Of the day’s active cases, 76 are recovering in one of the county’s five hospitals. Most are in Santa Maria’s Marian Regional Medical Center, a small number are in Lompoc Valley Medical Center, and the rest are in Cottage. Of all these, 22 are now recovering in an intensive-care unit. The highest number of patients that have been in the ICU is 25. At Cottage, three COVID patients are on a ventilator. Still, the number of new cases alarms medical professionals. They’re like dry tinder in the face of a coming forest fire. This Tuesday, the Public Health Department reported 184 new cases. That’s the second highest since tracking began.
What is the carrying capacity of the county’s medical infrastructure? The number of hospital beds, Dr. Fitzgibbons stressed, are only a small part of the answer. Hospitals don’t only treat COVID patients; people are getting sick and dying from many causes — many of which require a lot more than beds. Even so, beds are important.
Get the top stories in your inbox by signing up for our daily newsletter, Indy Today.
Fitzgibbons is a skilled clinician who happens to be comfortable communicating her complicated reality to the public. She took a few minutes out of her busy schedule to explain why some patients get sent home to recuperate, while others are put in hospital beds.
The first clue is breathing. “Our emergency room doctors are typically looking for shortness of breath,” she said. “And that’s subjective…. We want to see if they can speak with complete sentences.” Any patient who can’t becomes a candidate for a hospital bed. COVID-19 attacks the lungs’ ability to suck oxygen into the bloodstream.
The next thing emergency room doctors look for is a patient’s mental condition. “Do you seem confused? Are you less responsive? Are you more sleepy than usual? Do you exhibit signs of delirium?” This, she said, can be a sign of an oxygen deficiency. It can also be a sign of neurological problems, so the third test is whether the patient has experienced “any new or severe symptoms” — a sudden chest pain, for example. The list goes on. But blood oxygen levels are key. If a patient’s blood oxygen levels dips below 90 or 92 percent, that’s worrisome.
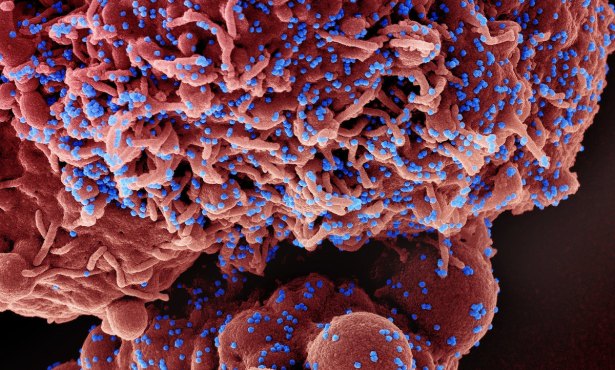
At that point, the patient might have a lung x-ray or a CT scan. These show whether the lungs are occluded. CT scans of COVID-infected lungs look milky and opaque, resembling broken glass. The thick white coloring around the outer perimeter indicates that the lung tissue isn’t getting the oxygen it needs.
COVID-19 also messes with other organs, including the heart. There can be neurological disorders. And blood clots in the lungs.
Not everyone who is hospitalized gets put into an ICU. Those are typically for patients who are very fragile or who are at risk of becoming so. The ratio of patients to nurses inside the ICU can be as focused as one-to-one. With no cure for COVID, care and treatment is essential. “If someone is that fragile, they need close attention,” Fitzgibbons said.
A typical stay for a COVID-19 patient in the ICU is up to two weeks. For those who stay out of the ICU? It is typically closer to four days.
At its worst, the body’s immune response to COVID-19 can unleash something called a “cytokine storm.” This is where the body tries to kill the virus and often winds up killing itself in a frenzied crossfire. Not all cases go that route. If they do, it usually happens within five to eight days after symptoms become apparent.
“We understand the disease much better now than we did four months ago,” said Fitzgibbons. Now, medical professionals are better able to anticipate and treat the complications. As with most diseases, it’s often the complications that kill you. “We are much better at taking care of severe pneumonias,” she said. Same with blood clots — which often present as microscopic blood clots on the lungs. Or as strokes.
Who gets put on a ventilator? Or more precisely, who has a ventilator put in them? This is a horrific, if amazing, medical intervention in which a patient is placed into an induced coma, sometimes turned on their stomach, and paralyzed so that the ventilator can breathe for the body. The survival rate for this is not high. Those lucky enough to make it, Fitzgibbons said, may report pulmonary issues as long as two months later. The recovery time for someone who is ventilated often lasts three to four weeks.
The nonstop question confronting medical professionals like Fitzgibbons is capacity. How many patients can a hospital treat? “That’s the conversation we have every day across the country, across the state, and across the county,” she said. “In Santa Barbara, right now, we have the capacity to take care of the disease,” she said. But what happens in three or four weeks? “We really don’t have much of a counterforce to change the trajectory of the caseload. The good news is that we have capacity, but it’s a complicated question.”
Are there enough doctors and nurses? Enough technicians and support staff? Does the hospital have enough capacity within its entire system to handle the load? A week ago, Cottage announced it was cutting back on elective surgeries to engineer more capacity into its system. But elective surgeries help pay a hospital’s freight. And elective surgeries, if postponed too long, stop being elective.
For Fitzgibbons, the hardest part has been the social disconnect the pandemic has inflicted. “We get used to living this really rich life where we know so many people who interact intimately with you: kids high-fiving each other, visiting grandparents, a weekend at the beach. To turn from all that can be devastating to the mental health of an entire community, to parents, friends, co-workers.” Making it harder still, she said, is the lack of “any fixed point in the future when it will be over.”
What gives Fitzgibbons hope? “We’ve demonstrated that we can bring the numbers down before.”
At the Santa Barbara Independent, our staff is working around the clock to cover every aspect of this crisis — sorting truth from rumor. Our reporters and editors are asking the tough questions of our public health officials and spreading the word about how we can all help one another. The community needs us — now more than ever — and we need you in order to keep doing the important work we do. Support the Independent by making a direct contribution or with a subscription to Indy+.