The Grim Truth of COVID-19
A Santa Barbara Doctor Speaks of the Suffering of Patients and Families
In December, the Santa Barbara Independent put out an open invitation to health-care workers who deal with COVID-19 patients to tell us their stories. The following is the first of those stories.
Most medical narratives involve high drama with scenes out of Grey’s Anatomy or ER. But drama is not the narrative of this pandemic; the reality is much more grim. The narrative of this pandemic is overwhelmingly one of suffering — the suffering of those sickened by COVID-19 and their loved ones.

I am a Hospitalist at Cottage Hospital, a specialist in Internal Medicine primarily responsible for the management and care of hospitalized patients, and right now most of these patients are admitted for complications related to the novel coronavirus.
Many perceive this illness as a binary affair, an ordeal that you either survive or you don’t. While the infected can have minimal or even no symptoms, for many, the illness is debilitating with weeks of severe cough and fevers, as well as muscle and joint pains.
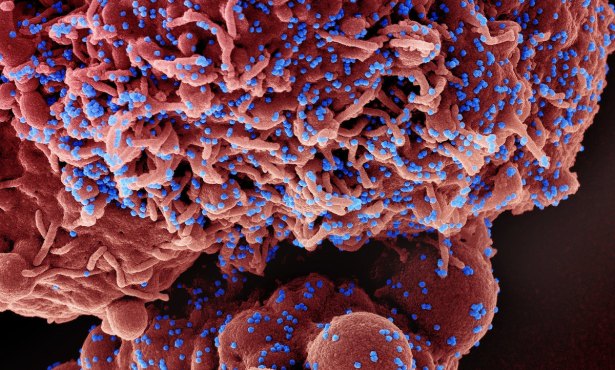
The virus triggers a robust inflammatory response that can result in long-term consequences as well. The list is long, reading like a pharmaceutical advertisement disclaimer: diminished lung capacity, blood clots to the lungs, strokes, heart disease, heart failure, arrhythmias, long-term and possibly permanent alteration of taste and smell, cognitive decline, and psychiatric disease.
COVID-19 can affect virtually all organ systems, but primarily infects and damages the lungs, impairing their ability to function. As a result, the majority of hospitalized COVID patients are admitted with pulmonary involvement — in the best cases, merely requiring supplemental oxygen, whereas in the most dire cases requiring mechanical ventilation. Medical management is primarily supportive, and we employ the limited therapies at our disposal in an effort to help the body heal itself.
Most COVID-19 patients require a prolonged hospitalization lasting weeks or months to allow damaged lungs to heal. For the duration of this hospital stay, they exist in this liminal space alone — their only contact to their previous life being the telephone or computer. Their isolation is punctuated only by visits from nurses, doctors, and cleaning staff — all gowned with masks, face shields, and caps.

These physical barriers are alienating and obscure the subtle social cues that humanize interaction. Most patients will improve and be discharged home or to a nursing home for further rehabilitation. Those who don’t will take their last breaths with only their nurse by their side.
Lungs absorb oxygen more efficiently when the patient lies in the prone position, so patients typically spend the majority of their time positioned on their stomachs. The sickest among them are moved to the ICU on a ventilator, a machine that pushes breath against their stiffened lungs through a tube inserted through their mouth.
Most of these patients have already been here for weeks, with potentially more ahead, before they improve, they succumb to their illness, or their care is deemed futile and treatments sadly withdrawn. The odds are that many of the sickest will not survive. The ones who do will be forever changed, weakened from their immobilization and facing months to years of intensive therapy to recover sufficient strength to function independently.
Some of these patients will even require tracheostomies — breathing tubes surgically placed through the front of the neck.
The virus is unpredictable. Patients can show improvement, even recovery, before deteriorating suddenly and unexpectedly. As physicians, we are reminded of the stochastic nature of our profession — that even with the best care, outcomes are uncertain. Despite our training, experience, and expertise, existential dread permeates the day, not knowing what tragedy will unfold before us. Unfortunately, this same experience is reflected in my colleagues’ accounts of battling this virus worldwide.
The usual outside impression of my work is that of saving lives and stamping out disease. In reality, much of my day is spent on the phone helping families navigate and come to accept illness and death as they watch their loved one’s previous life disintegrate. In doing so, we as physicians perform the emotional labor of compartmentalizing our own anxieties while attempting to promote realistic expectations about our patients’ futures — to help their families understand that the person they brought to the hospital lived in the past.
It is the nurses who ultimately bear greatest witness to this suffering. They are the ones who carry out the duties of care, attending to the large tasks and smallest details. And it is nurses who spend the most time in close contact with patients, placing them at the greatest risk for contraction. I cannot sing the praises of the nursing staff at Cottage Hospital enough. They are truly the ones on the front lines, and I am continually humbled by their skill and grace in the face of this relentless plague.
The hospital has become an entirely different world from the one outside its doors. It’s a disorienting experience on my commute to see close gatherings, as if from another era I remember from years ago.
For many people, the virus is something they only read or hear about, what Camus described as the “abstraction” in the early stages of The Plague. The fictional townspeople in his book had a sense of the illness slowly spreading in their midst, although without a direct connection to it, they carried on with their normal lives as usual. COVID, for many in our community, remains just such an abstraction. People can read the news and be awed by the number of cases, but until it enters their life directly, they will not appreciate the true misery the infection brings with it.
Denial and disbelief are normal human coping mechanisms. For many there is an unconscious assumption that their health or virtue will protect them — the “just-world” fallacy in practice. My patients come from all corners of the county and from all walks of life, with ages ranging from the third decade of life through the tenth. While severe disease and complications primarily affect the elderly and those with underlying illnesses, no one is immune.
This virus is absolutely everywhere; wherever you encounter groups of people, you are almost certain to be in its presence.
Most concerning to me about this pandemic though is the steady stream of scientific denialism that has accompanied it. Misinformation that downplays the severity of the virus has fueled attitudes that have allowed this virus to reach its current level of crisis and have led to violent attacks on health-care workers. It has influenced the behaviors of many of those suffering within our community and contributes to the misery I wade through on a daily basis. It would be nice to believe that it’s not that bad and we can continue our lives as we did before. This, of course, is wishful thinking.
This virus has extracted a cost, the depths of which we will only come to understand in the decades to come. Beyond the human suffering, economic consequences, and lifestyle disruptions, the real tragedy is the fact that the extent of this pandemic was at least partially preventable. When public health becomes politicized, public health fails.
Fortunately, Centers for Disease Control guidelines and a new vaccine have given us a way forward and the ability to mitigate the misery this virus brings. “Public welfare,” Camus wrote, “is merely the sum total of the private welfares of each of us.”
We all know how to turn this tide. The question is if people will change their attitudes and behaviors before they become personally impacted. In Camus’s parable, the plague comes for everyone eventually in one way or another.
Ben Diener, MD, is a physician board certified in Internal Medicine and has been practicing in Santa Barbara since 2006. A Santa Barbara native, he was named 2018 Santa Barbara Cottage Hospital Physician of the Year.
At the Santa Barbara Independent, our staff is working around the clock to cover every aspect of this crisis — sorting truth from rumor. Our reporters and editors are asking the tough questions of our public health officials and spreading the word about how we can all help one another. The community needs us — now more than ever — and we need you in order to keep doing the important work we do. Support the Independent by making a direct contribution or with a subscription to Indy+.


You must be logged in to post a comment.