If knowledge is power, a Pacific Pride Foundation–sponsored virtual town hall on Wednesday evening gave everyone watching and listening the power to avoid monkeypox and to gain a better understanding of the sometimes very painful disease. Moderated by Kristin Flickinger, executive director of Pacific Pride, the talk included Santa Barbara County Public Health’s Dr. Henning Ansorg, infectious disease specialist Dr. Lynn Fitzgibbons, Santa Barbara Neighborhood Clinic’s Dr. Charles Fenzi, UCSB’s Student Health medical director Dr. Erin Moore, and Planned Parenthood’s chief medical officer Dr. Maryam Guiahi.
Flickinger described the hurt and angry feelings that had arisen among the LGBTQ+ community about a disease that inevitably raised echoes of the deadly 1980s AIDS epidemic and how the United States ignored it for too long. Monkeypox is also an infectious disease that was having an impact on the community of men who have sex with men, she said, asking everyone to have conversations that were honest and avoided stigmatizing anyone. Was it fair to compare monkeypox to HIV in the 1980s? she asked.
Dr. Fenzi was the first to respond, stating that who they needed to reach was anyone who could be exposed. It wasn’t just a disease among men, he said. In California, 82 women were diagnosed with monkeypox, and around the nation, eight infants were diagnosed. He was concerned for caregivers, who needed to wear personal protection. And he agreed that this was indeed like the AIDS epidemic, which he recalled — making a benedictory sign of the cross — affected men and women alike, not just one group of people.
Monkeypox is a self-limiting disease, Dr. Guiahi pointed out, and is rarely fatal. She said a lot of credit went to the LGBTQ+ community for raising the bar and leading the charge on the need for information and action.
The medical professionals took turns answering questions from Flickinger and the audience, and a composite of their responses is grouped by topic:

What are the symptoms of monkeypox?
A patient typically has been exposed in the past one to three weeks. Their history alone will say a lot. They might notice flu-like symptoms: fever, muscle ache, swollen glands. People say they feel so sick, tired, or exhausted. After one to four days, a skin rash might occur on the hands, feet, chest, mouth, genitals, or anus. They can look like big pimples or large blisters. And it can look like herpes, so testing is important.
It takes about three to four weeks to really get better, the flu-like symptoms to end, the lesions to scab over, get less tender, and then resolve. People with weakened immune systems might have a more severe or prolonged case.
How is it spreading?
Monkeypox can be sexually transmitted, but it’s different from syphilis or gonorrhea. It’s spread by close mucosal or skin-to-skin contact, as in intercourse.
What should I do if I have monkeypox?
Most people have the flu-like symptoms at least one day before lesions show up. You should refrain from going out if you don’t feel well. Avoid cuddling or kissing if you’re coming down with something. Avoid body-to-body contact because you will spread the disease if you have it. You will be contagious until the lesions have healed and new skin has replaced the lesions. That can take weeks. This is a responsibility every individual can take.
[California’s new guidance on home isolation can be found here.]
How do you detect monkeypox?
A skin lesion can be swabbed and a test sent to the laboratory, where there are no bottlenecks. Any doctor, clinic, or hospital can send a sample to be tested.
How do you prevent monkeypox?
There are five confirmed cases in the Santa Barbara community, but this is undoubtedly the tip of the iceberg. If a partner has suspicious symptoms, this is a good time to be cautious and remember that there’s a lot more disease circulating than we’ve been able to confirm.
This is a good time to practice safer sex, to limit the number of partners, and to be forthcoming if you have skin lesions. You can also have a conversation and ask about symptoms or a rash.
Condoms are critically important, as are gloves or mouth shields. Mutual masturbation may be the way to go. Or remove yourself from intimacy if you think you’ve been exposed or if you have this disease.
Do you develop immunity after recovering from monkeypox?
Yes! That’s the good news, and it’s also why we don’t vaccinate people who have monkeypox. They are naturally immune.
However, the lesions can be extremely painful if around the eyes or urethra. Those cases, pregnant women, and people with certain skin conditions are considered high-risk cases and can get the vaccine, as well as the medication tecovirimat — or Tpoxx — if they develop a severe case.
Sign up for Indy Today to receive fresh news from Independent.com, in your inbox, every morning.
Is the vaccine effective?
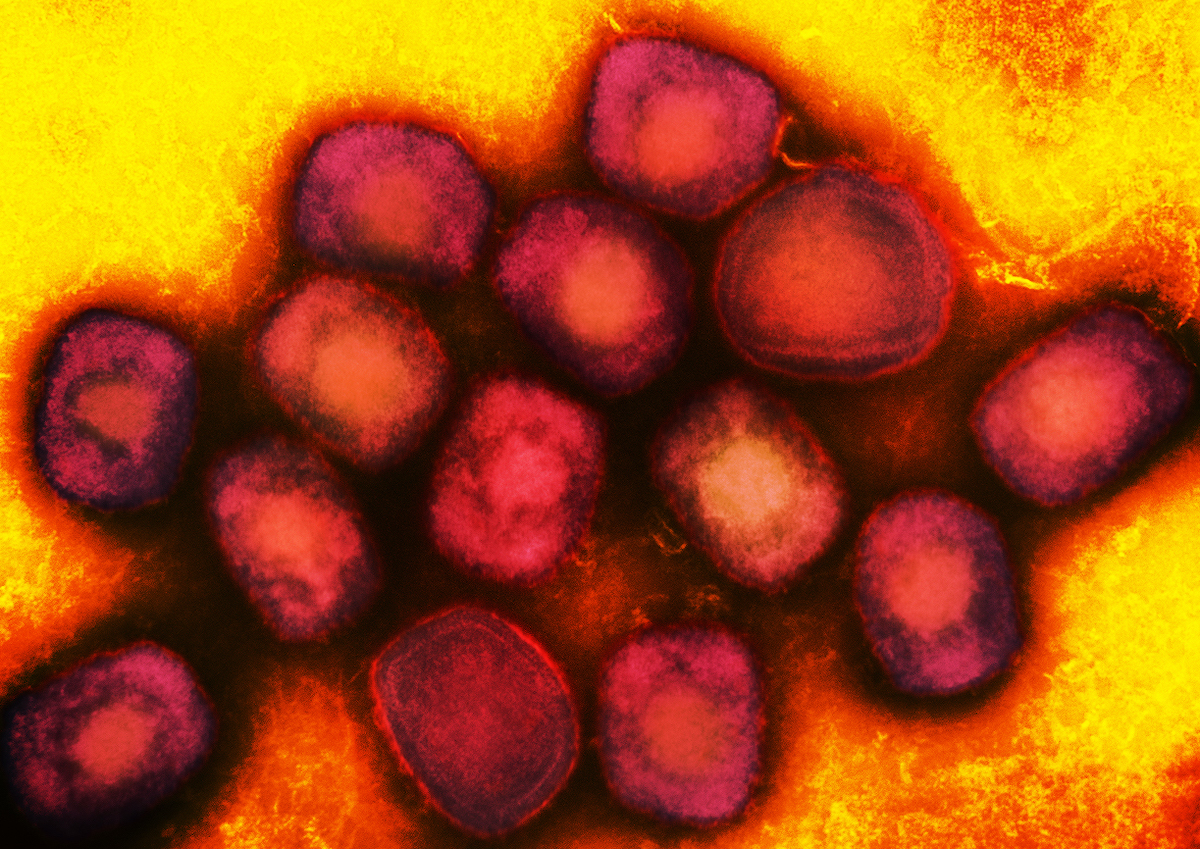
The monkeypox virus is in the smallpox family. The U.S. government has stockpiled medicines against bioterrorism threats, and the vaccine designed for smallpox works on monkeypox. However, it’s not medically authorized for monkeypox, so although it’s available, the paperwork is very cumbersome.
There are two smallpox vaccines. The Jynneos is preferred, because the other is a live virus vaccine with significant side effects.
And a previous smallpox vaccine — members of the Armed Forces were vaccinated in the early 2000s, for example — may offer some protection, though it varies from person to person, especially if it were as long ago as the 1950s.
Who can get the vaccine?
Unfortunately, the vaccine is scarce. Until more becomes available, the current supply — and Santa Barbara County has 1,000 doses — is limited to people who’ve been in contact with a confirmed case. Post-exposure vaccination can blunt monkeypox symptoms or decrease the risk of getting the infection. (The monkeypox vaccine is very different from the COVID vaccines, which do not work the same way.)
Santa Barbara recipients are limited to first doses until more vaccine becomes available. A first dose will protect up to 85 percent of cases; a second dose is better and gives protection for 10-20 years, but one dose will protect for the outbreak we are having now.
Also, you must be 18 or older to get the monkeypox vaccine.
In Los Angeles and San Francisco, where more vaccine is available, they are inviting people to be vaccinated who’d been at events where confirmed cases were found.
Pacific Pride Foundation and Planned Parenthood Central Coast are holding vaccine clinics — the next one is Thursday, August 25, in Santa Maria. Clinics that treat sexually transmitted diseases, emergency rooms, and UCSB Student Health are also being allocated a small supply.
Could a vaccinated person be a carrier and infect an unvaccinated person?
We don’t know enough at this point, but we are optimistic, thinking of parallels to other infectious diseases, that this vaccine is going to be very, very protective. Does that mean it will prevent someone from becoming transmissible? Hopefully more so than if they were not vaccinated. We want to be cautious in being reassuring, because the vaccine is not like a bulletproof vest.
Is there outreach ongoing to the Spanish-speaking community?
Yes, and we are thinking about how best to reach the Mixteco and Indigenous people and speakers, including having a tri-lingual Town Hall. Materials are produced in both English and Spanish, and Pacific Pride’s website is one quick translation.
Pride Fest Begins Soon
At the end of the forum, Flickinger noted that the Pacific Pride Festival events will begin soon, with the big outdoor festival on Saturday, August 27. She said that people understand that this can be transmitted through sex if someone has symptoms. “We know how to get checked out; we know how to take a pause. This is different from saying, ‘Don’t have sex.'” But with the Pride Festival coming up, what was the panel thinking about other ways of transmission? she asked.
Dr. Fitzgibbons made the point that it was important to separate what was well-established and known from what was making the rounds as an interesting but singular story. “It’s like the early months of COVID: People are anxious, but they don’t have a strong foundation in understanding the disease.
“With monkeypox, this disease does not seem to be spreading easily with short contacts or with aerosol droplets in a crowd. If that were the case, we’d be seeing a lot more clusters related to these types of scenarios. There have certainly been infectious people in these situations, but we’re not seeing big pockets of infection.”
The doctor said that the medical journal Lancet had reported a case in which monkeypox spread from people to a dog. The Independent spoke with Dr. Fitzgibbons later to ask her opinion of a report of an apparent case involving a man who had been dancing outdoors in a crowd.
“What’s already clear is that monkeypox is not spreading through aerosol droplets as efficiently as COVID had, for instance. There are not countless cases of spread from a surface like a doorknob or from an indoor meeting.
“When it comes to a festival like Pride, being close to people of unknown monkeypox status for long periods of time, that may bring some risk,” Dr. Fitzgibbons said. But the case involving a dog and the one about a man at a dance, those were just one or two drops of information in a big ocean of case reports.
“We’ll know much more three months from now, but walking around at the Pride Festival next week? I am not fearful of catching monkeypox in that crowd,” said Dr. Fitzgibbons.
To view the virtual town hall, click here.
The vaccine clinics are currently limited to close contacts of infected individuals, and only people ages 18 or older may be vaccinated. Check with Santa Barbara County Public Health Department at (805) 681-5280 or PHDDiseaseControl@sbcphd.org to verify eligibility. The vaccination clinic in Santa Maria takes places on August 25, 5-8 p.m., at 105 North Lincoln Street. More information is available at Pacific Pride’s website.
Support the Santa Barbara Independent through a long-term or a single contribution.


You must be logged in to post a comment.