Likely Suspects in Cancer Growth
Stem Cells Seem to Play Key Role
Recently, a link was discovered between two widely studied medical areas: cancer and stem cells. Cancer stem cells, as their name implies, are stem cells that have been found within cancerous tumors.
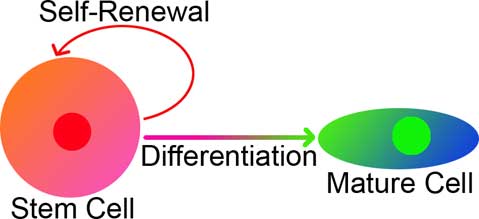
When you understand stem cells, it quickly becomes apparent why they might be in tumors. Cancerous tumors are a mixture of many different cell types. If the tumor is originally from one cell gone bad, that single cell must be able to become different types of cells; a key defining characteristic of stem cells is that they can become multiple different cell types, a process called “differentiation.”
Another central trait of malignant tumors and stem cells is their proliferative ability: tumors can grow out of control, while stem cells, by definition, can “self-renew,” or create more stem cells.
These two shared traits make the stem cell a very likely suspect for playing a key role in cancer, and led to the theory of cancer stem cells (CSCs). CSCs have been broadly defined as cells within a tumor that can become other cells (creating the heterogeneity seen in tumors), and can self-renew (regenerating the CSC population).
In order to comprehend how cancer stem cells are created, it is important to understand the theories behind the creation of cancerous tumors. Cancer can occur when mutations have accumulated in certain genes. The genes usually mutated in a cancerous tumor are (1) oncogenes, which control cell growth, and (2) tumor suppressor genes, which make sure the cell retains its cell type (i.e. a liver cell does not become a brain cell). These genes are often mutated in CSCs.
A mutation in a gene that normally regulates cell growth can cause that cell to quickly increase in numbers. With a large population of mutated cells, there is a greater likelihood that a second mutation can occur than within a small population of cells; when enough mutations accumulate in a cell, it can defeat the normal cell growth restrictions so thoroughly that it grows out of control, becoming cancerous.
Although the cancer stem cell theory developed in the 1970s, recently it has gained a spotlight in the scientific community. The first functional identification of CSCs was in 1997 in acute myeloid leukemia. Researchers found that although tumors are made up of many different cell populations, there was only one population capable of generating the tumor. This was determined by taking a tumor and breaking it up into its many different cell types and then injecting each separately into mice; one group of cells, the CSCs, could recreate the original tumor, including the shape and specific cell types found in the original. It has been found that CSCs account for only a small percentage of the total number of cells in the tumor, varying from as little as 0.002 percent to around 30 percent, depending on the type of tumor, but it seems to be usually less than 10 percent.
Cell Markers: The different cell populations within a tumor can be separated and identified by the proteins they make; cells creating the same sets of proteins can be grouped into one population. Because such proteins are commonly used to identify and categorize cells, they are called cell markers. CSCs from the same type of tumor make the same set of markers.
(The CSCs in multiple cancer types may make the same cell markers, though. For example, CSCs found in pancreatic cancer produce a cell marker called CD24. However, CD24 is not made by all CSCs; breast cancer CSCs do not produce CD24, but do produce another marker called CD44. Interestingly, CD44 is also made by CSCs in pancreatic cancer and several other cancers: ovarian cancer, head and neck squamous cell carcinoma, and probably others. Another cell marker found in many different tumor types is CD133; CSCs in malignant tumors of the brain, prostate, colon, lung, and liver have it.)
However, these cell markers are not found exclusively in cancerous tumors; these markers are often in stem cells in normal, healthy tissue and do not pose any apparent malignant threat. Stem cells from the brain, intestinal lining, and other tissues, all make the marker CD133. CD44 is produced by mesenchymal stem cells (in muscle, connective tissue, fat, and fetal liver and lungs) and bone marrow stem cells. It’s becoming clearer that some CSCs have the same markers as normal stem cells in the healthy tissue of the tumor origin.
It’s unclear what the implications of this might be. However, surprisingly, sometimes CSCs produce cell markers different from the normal stem cells in the healthy tissue. These CSCs may be migrating from another tissue to the tumor site, or, alternatively, the CSCs may be mutated stem cells that resided in the original, healthy tissue. Because CSCs can become other cell types, they could change which cell markers they produce; CSCs may make a set of markers very different from the cells they were before residing in a cancerous tumor.
As more evidence is reported pointing at the key role of cancer stem cells in the creation of cancerous tumors, it becomes more crucial for researchers to have a thorough understanding of these stem cells. Although the CSC populations can be identified by different cell markers and their ability to create tumors in a mouse model, there is still much about them that is not well understood: how they are created, how their origins are related to non-cancerous stem cells, and whether they are present in all cancerous tumors. As more answers come to light, researchers will be able to answer the most important question: How can we use our knowledge of CSCs to most effectively combat them?
Further Reading
Rowland, Teisha. “Cancer Stem Cells: A Possible Path to a Cure.” AllThingsStemCell.com. 2009.
Biology Bytes author Teisha Rowland is a science writer, blogger at All Things Stem Cell, and graduate student in molecular, cellular, and developmental biology at UCSB, where she studies stem cells. Send any ideas for future columns to her at science@independent.com.



