Santa Barbara COVID Cases and Hospitalizations Keep Going Up, Up, Up
But Health Facilities Are Still Well Below Capacity, Officials Say
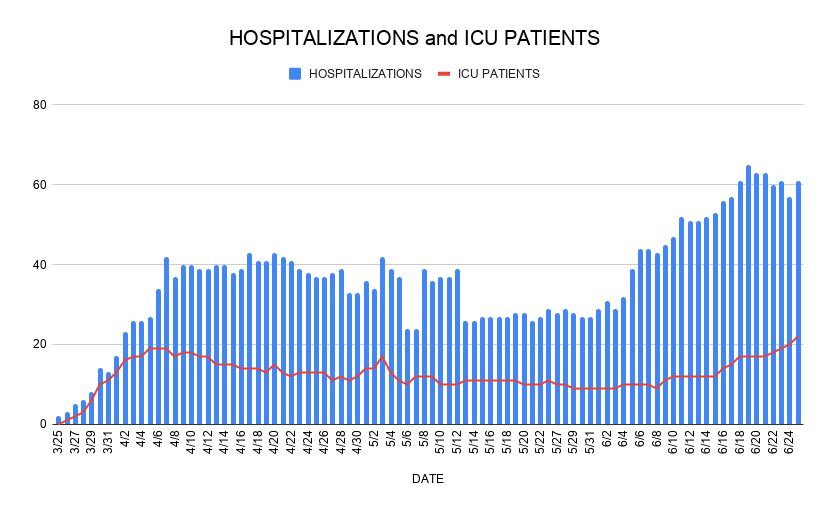
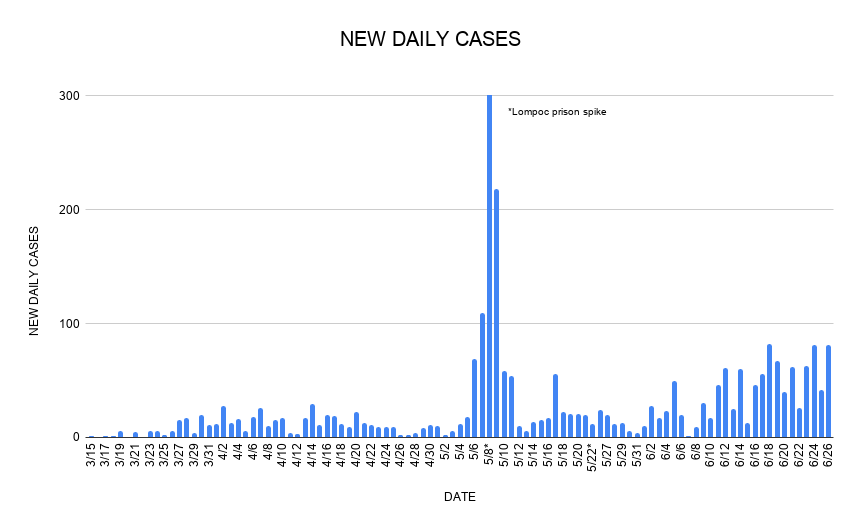
Yes, COVID-19 cases are steadily increasing in Santa Barbara County, Supervisor Gregg Hart admitted Friday. “It’s not good news,” he said, “but frankly, it was not unexpected,” given the region’s recent transition from total shutdown to rapid restart. Hospitalizations have consistently risen over the past month, data shows, and ICU patients peaked this week at 22, the highest number since the coronavirus first reared its head here in March. Six people died over the last seven days.
However, Hart went on, overall active cases are actually on a decline ― from 315 last Friday to 254 this Thursday ― and Santa Barbara County’s hospitals are in no danger of being overwhelmed. In fact, he explained, COVID-19 treatment beds are occupied at only 8.7 percent of available capacity and surge beds are only 6.9 percent full. ICU beds are operating at 16.8 percent capacity.
Hart acknowledged the seeming incongruity of reopening personal care businesses like nail salons and tattoo parlors, which the Public Health Department just allowed, while case counts keep going up. But according to local and state data, he went on, “The very small, incremental contribution of the reopening of personal care service businesses will have on future COVID-19 cases is not a serious threat to public health in our county.” Most of the community spread, Hart said, is coming from interactions between family members, coworkers, and friends.
To keep the continuing outbreak as manageable as possible, residents ought to maintain physical distancing, wash their hands often, and wear face coverings, Hart said, noting Governor Gavin Newsom’s new order mandating face masks in public places. “We want to reopen businesses, we want to give people the opportunity to maintain their livelihoods, and we want everyone to stay safe by being diligent and careful,” he said.
Dr. Henning Ansorg, the county’s Health Officer, agreed that the rising case count is “concerning to us.” But he also explained that the increase can be partially explained by expanded testing capabilities. Many of the new cases are asymptomatic, he emphasized, and most patients who actually get sick don’t require hospitalization. “When comparing the increase in new COVID positive results to the increase in hospitalizations, it is obvious that the relative increase in hospitalizations is in fact slightly lower than May, percentage-wise,” he said.
Ansorg reiterated that community transmission is taking place among family units as well as friend and work groups. “The vast majority of new cases get infected by someone they know,” he said. And, like Hart, he underscored the importance of face masks and social distancing. “We cannot stress enough these simple preventative measures,” he said.

Sheriff Bill Brown offered an update on the growing outbreak at the County Jail. Eighteen staff have now tested positive, including the jail’s chief custody deputy, Brown said. That’s up from nine last week. Three inmates are infected and are all being treated on-site. So far, 322 employees and 155 inmates have been tested, with more testing on the way, Brown said.
Meanwhile, after weeks of encouraging residents to get tested at community testing sites, officials are now asking people to make an appointment only if they have symptoms or have been exposed to the coronavirus. Nick Clay, director of the county’s Emergency Medical Services Agency, said there’s been a bigger than expected demand and are supplies are running short.
“We want to reinforce that these testing opportunities are not a cure for curiosity but for those who have had a risk of being exposed,” Clay said. “What we are finding is that the ‘worried well’ individuals are coming in a volume that prevents individuals who do need the test.”
Some public testing sites now have up to a 10-day waiting list, Clay said. The turnaround time for results has increased from two or three days to five days.



You must be logged in to post a comment.