In the COVID-19 Trenches with Santa Barbara’s Dr. David Zisman
The Sansum Pulmonologist and His Team Are Fighting the Good Fight

Dr. David Zisman is a pulmonary and critical care medicine specialist. He’s seen a lot over his career, which took him from Venezuela to Texas to Santa Barbara. But he’s never seen anything like this. “This is a new disease for us,” he said, “a new infection. We have no previous experience, and there is very little scientific information to go by.”
Zisman is one of eight pulmonary doctors tending to some of the county’s sickest COVID-19 patients. (Four work for Sansum Clinic, four work for other providers.) It’s been a long few weeks with more tough days ahead. But Zisman and his colleagues aren’t about to give up. Not by a long shot. And while they’re not looking for recognition, they certainly deserve it.
Zisman took time between shifts this week to speak with the Independent. Our exchange has been edited for length and clarity.
How are things right now, and how do they compare to mid-March, when the coronavirus first reared its head in Santa Barbara? In early April, things changed for the better. The hospital had created two ICU units devoted to COVID patients. Another huge improvement was the turnaround time of tests [for critical patients]. It used to be four to five days on average. Patients would have to stay in the ICU until we knew for sure what they had. That was stressful. I worried we would run out of ICU beds. But now we are able to perform testing in the hospital, and it only takes a few hours to get the results. That’s allowed us to move patients out of the ICU appropriately.
What is your day-to-day like? In general, [the pulmonary specialists] have kept the same scheduling structure. We each do a week of attending in the ICU, and there are typically two specialists rounding on every single patient. We also have scheduling recommendations to the hospital for a possible surge. We are seeing more COVID patients than regular critically ill patients, in large part because of the pandemic. But also because elective procedures have been canceled.
What is the experience of trying to treat a completely novel virus? There has been tremendous anxiety. And there is a lot of hype and information out there that is sometimes biased or coming from unreliable sources. But certain aspects of this virus we do recognize and have seen before. We are still trying to define best practices and determine the underlying injury and response patterns that these patients are displaying. There are still a lot of unknowns.
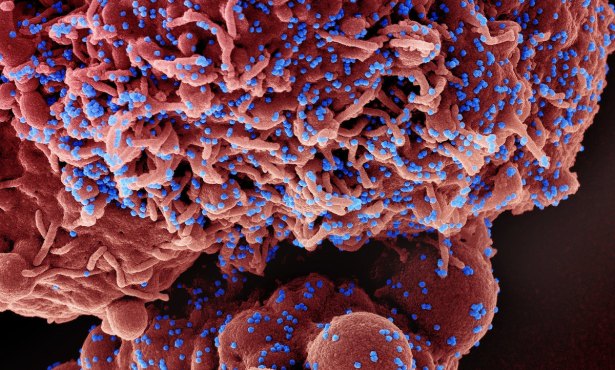
What actually happens to a person’s body and lungs when they are infected with COVID-19? We are starting to see data from China and other places that is helping us understand it a little better. In debilitated patients, the virus injures the linings of airways and the lungs’ air sacs. This produces a brisk immune response. In some cases, this natural immune response can cause injury to the patient. It appears from some autopsy studies that it may also hurt blood vessels. This is a potentially new or unique way this virus causes harm, one we have not seen before. Having this information can impact how we recognize and treat this condition.
What are you and your colleagues doing to keep yourselves safe? There is a significant safety protocol for health-care workers entering the ICU and going into patients’ rooms. A lot of [protective personal equipment] is used, and we know how long we can wear each item. Under normal circumstances, we don’t usually gear up like this. We are monitoring ourselves very closely. I’ve been sleeping in a different room than my wife and staying away from my children. We are using separate dishes, etc.
This is a very difficult time ― especially for you and your patients ― but have you seen any silver linings? This experience has really united the field. It’s amazing how pulmonologists, respiratory therapists, and nurses have become like one unit. We are sharing information with each other, making sure we are protecting each other. To see how we can come together when we’re faced with a common threat, that has been really uplifting. We also see that in our communities and around the world. We are forgetting our political and cultural differences and remembering we are all humans who we need to support each other.


You must be logged in to post a comment.