Surge in COVID Cases Strikes Skilled Nursing Facilities
Santa Barbara County’s Post-Holiday Spike Affects Senior Care Homes
The calendar doesn’t lie.
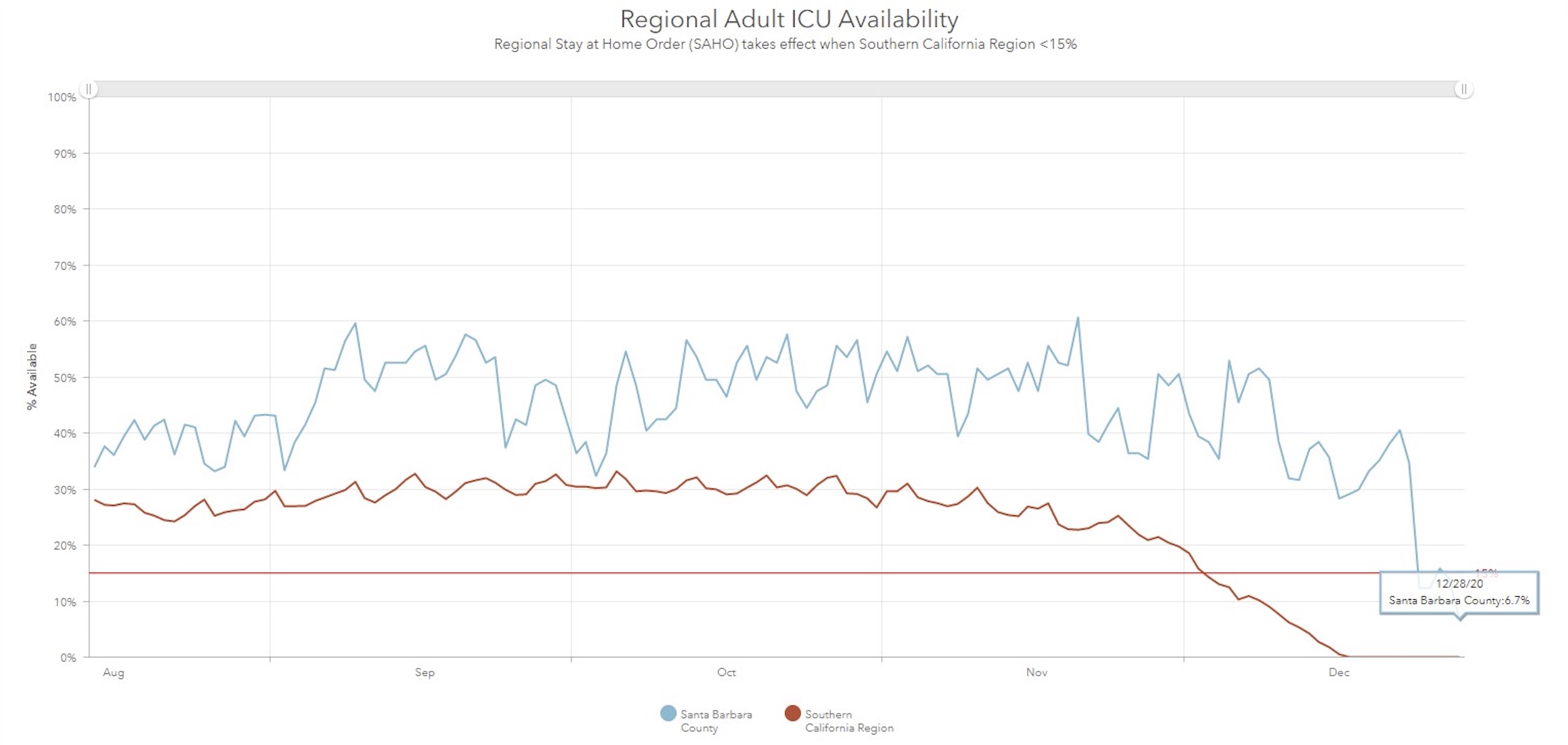
Four weeks after Thanksgiving, hospitals began hitting their peak COVID patient-load since the pandemic began — an increase that public health officials in Santa Barbara County attributed to traditional holiday dinner parties. Santa Barbara’s intensive-care unit (ICU) bed count dropped to 12.3 percent over Christmas and on Monday hit 6.7 percent, its lowest yet. The Southern California Region has been at zero ICU capacity since December 17, and its worst-hit area, Los Angeles, faces COVID patients in hospital common areas and freezer trucks in the back bays for bodies.
Although Santa Barbara County is not testing for the presence of the new B117 variant of the coronavirus — a mutated SARS-CoV-2 virus first identified in Great Britain and considered more contagious than the original virus — it requires congregate-care facilities to test all staff and residents every week. Older residents remain vulnerable to the highly transmissible disease, and a situation report stated the county was investigating outbreaks at 53 facilities.
Among them is Buena Vista Care Center. “For months there were no new cases, and it seemed the worst was over,” said Christina Eliason, whose father lived at the skilled nursing facility for two years. She told the Independent that Buena Vista had held an earlier outbreak to seven residents, one of whom died, after 24 staffers were stricken. “Now we’re seeing the ‘post-Thanksgiving’ California surge rage like wildfire through the facility,” she said.
Eliason noted that posts on Buena Vista’s COVID page indicated 13 residents and 11 staff members had tested positive between December 22 and 26. Her father tested positive December 22, and he died on Sunday.
Get the top stories in your inbox by signing up for our daily newsletter, Indy Today.
“Just last week, we received notice that they would begin administering the new vaccine, but he did not get his first dose before falling ill,” Eliason said. “The vaccine is tragically mere days too late for the many vulnerable residents who’ve just become infected.” Far from faulting Buena Vista, Eliason said her family was grateful to its compassionate staff and the vigilant nurses who cared for the COVID patients around the clock, isolated from the rest of the facility.
At Mission Terrace convalescent hospital, employees and residents succeeded in keeping the virus at bay until December 7. “We worked so hard, and we were so proud we were able to keep everyone safe,” said Eve Murphy, the facility administrator. That record was broken when two residents and a worker tested positive; Murphy stated the residents likely caught COVID while on an outpatient visit and that the worker was absent from Mission Terrace for two weeks before testing positive; all had recovered. The 60 residents and 78 staffers were to get a Pfizer shot on Wednesday, Murphy said, and Walgreens would be furnishing the vaccine.
Governor Gavin Newsom announced on Monday that the Pfizer vaccine would go to residents and staff at long-term care facilities through the pharmacies at CVS and Walgreens. The program came from the federal COVID-19 Pharmacy Partnership at no cost to state or local governments. Over three to four weeks, first nursing homes, then assisted living, residential care, and other long-term care facilities would receive the vaccine.
At Casa Dorinda, vaccinations started on Tuesday. CEO Brian McCague said CVS contacted the facility and set up a two-day schedule to cover the roughly 600 people at Casa Dorinda. Though McCague also has 18 employees who tested positive for COVID — but no residents — he had his doubts about the test.
One employee who tested positive was so extremely COVID-conscious that McCague had the test repeated — twice. Each time, it was negative. McCague has had other employees’ tests repeated because he knew how extremely careful they were: “I’d say our false-positive result is much higher than the national average.” False positives haven’t been studied as much as false negatives, but they are believed to be less than one percent of all PCR tests — the nasal or throat swab tests. Dorinda’s 290 employees are tested once a week, and several could fall within those parameters over time.
McCague is not alone in his doubts about testing and the reports generated from tests. Several of the facilities contacted were puzzled or alarmed at the current cases or deaths listed for them by public health at the state and county level. “I am not sure where you obtained information to the effect that there are presently 14 COVID employees,” said Najib Yamak, “but that is not accurate.” Yamak runs Alto Lucero/Channel Islands Acute Care, and he has just one staff member out sick with coronavirus and three residents who tested positive. The vaccine is set to arrive on December 30, Yamak said.
Senior care facilities are of course high on Public Health’s radar because of the vulnerability of the elderly to the pneumonia and other issues that develop from COVID, and it is often seniors who enter intensive-care units. Santa Barbara County dropped into California’s ICU red zone of 15 percent on December 24, in part because Cottage Health revised its total capacity to reflect 45 staffed beds as opposed to 65 licensed beds. The other part was the increase in ICU cases across the county’s three hospital systems — from 21 on Christmas Eve to 26 on Christmas Day and 29 yesterday.
Hospitalizations don’t lie.
Cottage Health reports its COVID cases every weekday and has seen a steady creep since Thanksgiving’s single-digit COVID case load to 60 confirmed cases as of December 28. Fifteen people are in the ICU, eight of them on a ventilator, as of Monday. Marian Regional Medical Center reported case numbers remained consistent, but some COVID patients’ status had worsened and ICU intake was up over Christmas. Lompoc experienced a lower than normal case count, having one COVID patient in the ICU over the holiday. Staff and residents at the hospital’s Comprehensive Care Center skilled nursing facility would be vaccinated by the end of the week, CEO Steve Popkin stated, at least those who consented.
Consent to be vaccinated has also cropped up at a small skilled nursing facility called The Californian of Santa Barbara. Administrator Edgar Lopez said that among his staff, “Some are not 100 percent sure yet.” He noted, “They have every right to refuse,” adding that it was their right and he had to allow it.
For the most part, enthusiasm was high at The Californian. “We are ready to go with the vaccinations,” Lopez said cheerfully. The Californian has existed since 1963, and Lopez, though he would not say how many, acknowledged he had at least one resident ill with COVID. The first round of vaccinations would be on January 4 through Walgreens, Lopez said, and then they’d be back in 21 days for the second dose and to catch anyone they missed the first time.
His staff was “very conscious about what’s going on out there,” Lopez noted. On a daily basis, they are reminded of the COVID protocols for safety and encouraged to practice the same procedures at home — and this includes after being vaccinated. “The virus is something unknown,” he said. “A small amount of contact or exposure could still mean catching it.”
Every day, the staff of the Santa Barbara Independent works hard to sort out truth from rumor and keep you informed of what’s happening across the entire Santa Barbara community. Now there’s a way to directly enable these efforts. Support the Independent by making a direct contribution or with a subscription to Indy+.


