Stem Cells That Treat Leukemia, Lymphoma, HIV
Hematopoietic Cells Can Become All Different Blood Cell Types
Hematopoietic stem cells (HSCs), cells that turn into blood cells, have been heavily researched for decades, and have been successful in treating blood-related diseases in humans, such as leukemia and lymphoma, for much of this time. Recently, they were even successfully used in treating a patient with both leukemia and HIV.
Like many significant findings in science, their discovery was not made in search for such cures, but it was stumbled upon while dealing with another serious medical issue of the time: radiation exposure. During and immediately following World War II, scientists tried desperately to treat people who had been exposed to lethal doses of radiation. Transplants of spleen and bone marrow tissue were found to rescue these victims. It was later found that HSCs present in these tissues were behind these healing properties; researchers discovered this by lethally irradiating rats and mice and similarly rescuing them with transplants of different types of cells. The formation of the National Marrow Donor Program in the 1980s greatly increased the availability of these cells for research. HSCs have been successfully used clinically in humans since the 1950s, and to this day they are one of the few adult stem cells widely used in clinical therapies.
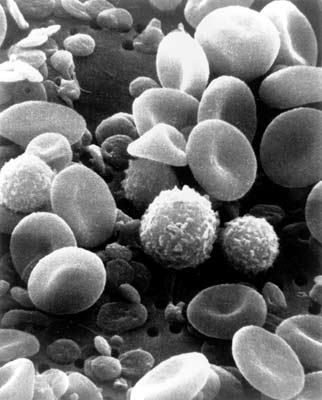
Hematopoietic stem cells are able to become, or “differentiate” into, all of the cells in the hematopoietic system. The hematopoietic system includes all the different kinds of blood cells, from myeloid elements (including red blood cells, white blood cells, and platelets) to lymphatic elements (such as T cells). These tissues are some of the most rapidly dividing cells in the body, and as such are generally the first cells hurt by radiation. For this reason, therapies using HSCs allows replenishment of the cells most damaged after exposure.
It is possible to isolate HSCs from a wide variety of both adult and fetal human tissues, including adult bone marrow, fetal liver, spleen, and thymus, umbilical cords, and blood. In recent years, there has been a great shift toward obtaining HSCs mainly from blood, using a much simpler and less controversial procedure. However, collecting a large enough number of HSCs for successful transplants remains a challenge.
It’s now not only better understood how HSCs from a donor can save a lethally irradiated recipient, but also how HSCs can be used in many other medical applications. HSCs are now being used to treat cancers of the hematopoietic system (leukemia and lymphomas), replenish cells lost to high doses of chemotherapy, and fight against autoimmune diseases, in addition to other medical applications.
Recently, an amazingly successful application of HSC therapy was used to treat a patient with both leukemia and human immunodeficiency virus (HIV). Under the guidance of Drs. Eckhard Thiel and Wolf K. Hofmann (at the Department of Hematology, Oncology, and Transfusion Medicine, Charite Universit¤tsmedizin, Berlin, Germany), doctors gave the patient special HSC transplants; amazingly, the patient had remission of both conditions after the treatment. As mentioned, HSCs have been used in transplants to rescue patients with leukemia, but this method had not previously been as successful for treating HIV, the virus that causes acquired immunodeficiency syndrome (AIDS).
In order to understand how the HSC transplant may have “cured” AIDS in this patient, it’s important to understand how HIV invades the body on a molecular level. Once in the body, HIV primarily attacks the immune system, including the T cells. However, some individuals have T cells that are naturally resistant to HIV infection. Over a decade ago, this resistance was found to be due to a mutation in a protein that is normally on the surface of T cells (called chemokine receptor 5 [CCR5]). This protein is thought to normally be involved in causing an immune response to infection, though its full function is still not understood. The HIV virus normally must interact with CCR5 in order to gain entry into the T cell. However, in individuals with a mutated version of CCR5, the protein is not functional and consequently does not allow HIV to enter the T cells.
The CCR5 protein has been greatly studied since its discovery, as it has been looked upon as a potential cure for HIV. Approximately 5 percent to 14 percent of Europeans have the mutated version of this protein, but it is absent in African, East Asian, and Native American populations. The mutation is thought to have arisen more than 5,000 years ago. Surprisingly, individuals with two mutated CCR5 copies have no apparent health problems. Anti-HIV drugs have been created that bind the normal CCR5 protein, attempting to block HIV entry into the T cells.
The recent success story that applied this knowledge of CCR5 and HSCs, mentioned above, was reported in February 2009. A 40-year-old Caucasian patient with leukemia and HIV underwent HSC transplants using blood from a donor with (two copies of) the mutated CCR5 protein. (This means his body underwent irradiation treatment to kill his existing HSCs, and these were then replaced by the donor’s HSCs.) Over 20 months later, not only did the leukemia go into complete remission, but the patient had no HIV detectable in his body either. As happens in treating leukemia, the donor HSCs replaced his irradiated immune system, but in this particular case this also meant that the normal CCR5 proteins on his T cells were replaced by CCR5-mutated, HIV-resistant T cells.
While this is quite the success story, a stem cell transplant like this, which involves risky irradiation of the patient, is still usually a less safe prospect than using well-developed HIV therapy drugs, though this could change with additional research. This treatment should be repeated in other patients to confirm the validity of the technique, and it must also be taken into consideration that some HIV strains do not access T cells using CCR5, but use other surface proteins instead.
This success, however, highlights the fact that while HSCs have been clinically used and studied to a large extent relative to other human stem cells, a great deal of work remains to be done to fully understand their molecular interactions and potential in medicine.
For more on hematopoietic stem cells, see Teisha Rowland’s “All Things Stem Cell posts on “Hematopoietic Stem Cells: A Long History in Brief,” or on Potential of Stem Cells to Cure HIV, or the National Institute of Health’s chapter on Hematopoietic Stem Cells, or, for a visual explanation of terms used, see All Things Stem Cell’s Visual Stem Cell Glossary.
Biology Bytes author Teisha Rowland is a science writer, blogger at All Things Stem Cell, and graduate student in molecular, cellular, and developmental biology at UCSB, where she studies stem cells. Send any ideas for future columns to her at science@independent.com.



