Cancer Vaccines: Part I
Field Is in Beginning Stages
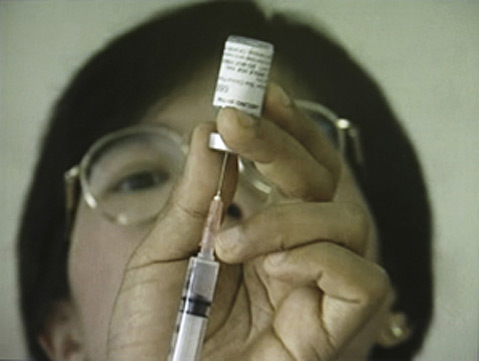
Cancer treatments today involve an astounding array of drugs. Often these drugs, such as ones used in chemotherapy, have a wide variety of negative side-effects, including fatigue, pain, and hair loss, to name just a few. An emerging, appealing alternative is vaccines against cancer.
While the field is just in the beginning stages, cancer vaccines hold great potential as a possibly more effective, and less detrimental, approach to treating cancer by working with the body’s own natural immune system.

In many ways, a cancer vaccine works very similarly to a normal flu vaccine. For both vaccine types, a “foreign” material enters a patient’s body in order to create a strong immune response against the material. The vaccine itself contains some part of the foreign material that will let the body identify the invader, such as parts of proteins and cells, or even entire cells. When your body is exposed to anything foreign it wants to expel, there are generally three main steps that take place to cause a full-on assault against the invader:
First, the body must identify the material as being “foreign,” an invader in the body. T cells, a type of immune system cell, accomplish this.
Second, the body must generate an immune response against the invader, which is in the form of antibodies (produced by B cells).
Third, rallied by the T cells, the body must strengthen the immune response against the invader.
In the field of cancer vaccines, there are two main groups of vaccines: “preventative” vaccines and “therapeutic” vaccines. While cancer is not what is typically thought of as an “infection,” evidence has shown that some cancers can be caused by infectious viruses. And so, preventative cancer vaccines have focused on vaccinating people against these potentially cancer-causing viruses. Again like the usual flu vaccine, preventative cancer vaccines are given to patients before they are infected, the goal being to prepare the immune system for a real, future attack. Remembering its encounter with the vaccine, the immune system should have a head start on producing antibodies for any real encounters with the virus in the future, preventing infection from even getting a foothold.
Therapeutic cancer vaccines, on the other hand, are for patients who already have cancer. Their aim is to prevent the progression of the cancer (e.g. reduce tumor size and the spread of the cancer) by stimulating an immune response against it. While some therapeutic cancer vaccines have had promising results, preventative cancer vaccines have been more successful.
The rest of this article will focus on preventative cancer vaccines, while therapeutic vaccines will be explored next week.
To date, preventative vaccines against two potentially cancer-causing viruses, hepatitis B and the human papillomavirus, are the only cancer vaccines approved by the FDA.
Hepatitis B (HBV) is a virus that causes about 80% of all liver (hepatic) cancers. (The other 20% are thought to be caused by alcohol consumption, obesity, and other conditions.) While liver cancer is around the fifth most common cancer globally, it comes in third for its resultant fatalities.
HBV can be easily transmitted through sexual contact or other exchanges of blood or fluids, such as through dirty needles or childbirth. The HBV virus attacks the liver specifically, causing it to become inflamed, although a person with HBV may not show any symptoms outwardly. Chronic HBV infection can lead to liver cancer. Just like the flu, there are different strains of HBV, and recent research has shown that some strains may be more likely to cause liver cancer than others. Fortunately, there are vaccines for HBV that can prevent viral infection, and consequently the development of liver cancer from it.
Effective HBV vaccines were approved by the FDA in 1981. The virus had been suspected for decades before this to cause liver cancer. The HBV vaccine was the first FDA-approved cancer vaccine. Today, there are two main HBV vaccines: Recombivax HB, made by Merck, and Engerix-B, created by GlaxoSmithKline. Both HBV vaccines contain part of a protein found on the surface of HBV, stimulating the body to build up an immune response against this piece of protein, to prevent infection with the virus. (Rest assured, it is impossible to contract HBV from vaccines like this.) HBV vaccines are now quite established and most children in the U.S. are vaccinated at birth. Great efforts have been made to establish at-birth HBV vaccination in areas where HBV is particularly prevalent, such as sub-Saharan Africa or Eastern Asia where over 80% of the global HBV infections occur.
Fifteen years after the FDA approved the HBV vaccine, the second, and currently only other, cancer vaccine was approved. It was for the human papillomavirus (HPV), which can cause cervical cancer. Every year, HPV infects around half a million women and kills around a quarter of a million women globally (including 4,000 deaths in the U.S.). It is transmitted through sexual contact and is extremely prevalent; it’s estimated that around half of all sexually active men and women get HPV at some point in their lives, and about 20 million Americans currently have HPV, though most may never know it. Like HBV in the liver, a persistent cervical infection of HPV, which may or may not show clear symptoms, can lead to cervical cancer.
In June 2006, the FDA approved HPV vaccines for girls and women ages nine to 26. The two HPV vaccines (Gardasil and Cervarix, again made by Merck and GlaxoSmithKline, respectively) very effectively protect against different HPV strains that cause cervical cancer. Early trials showed it to be nearly 100% effective in young women. Like the HBV vaccines, the HPV vaccines contain parts of proteins found on the surface of the virus, stimulating the body to recognize and attack the virus itself if it should encounter HPV. It is recommended to administer the vaccines to girls between the ages of 11 and 12, long before any potential exposure, but women up to 26 may also benefit from vaccination.
There are several other types of cancers known or suspected to be caused by viruses, though no vaccines currently exist for these viruses. For example, strains of the Epstein-Barr virus (which causes mononucleosis, commonly known as “mono”) are linked with several types of cancers: Burkitt’s lymphoma, gastroadenocarcinoma, and nasopharyngeal carcinoma. The Epstein-Barr virus (EBV) is thought to infect over 95% of people at some point in their lives. No vaccines currently exist for EBV, but some are in clinical trials and may one day prove an effective defense against not only EBV, but these cancers as well.
Although the idea of having a vaccine against cancer seems like science fiction, these vaccines are already here and, in the case of HBV, have been here for decades. However, these treatments currently only apply to the limited group of cancers that are caused by viruses. It has proven much more difficult to create successful therapeutic cancer vaccines that help a patient who already has cancer. But despite great difficulties, therapeutic cancer vaccines have already made it to clinical trials for a variety of cancers, including lung, breast, prostate, colorectal, melanoma, lymphoma, and kidney cancer. Some of these vaccines have had very promising results, and these will be the focus for the next “Biology Bytes” article, Cancer Vaccines: Part II.
For more on cancer vaccines, see the U.S. National Institutes of Health: National Cancer Institute’s fact sheet on cancer vaccines, including a list of active clinical trials of cancer vaccines, their fact sheet on the HPV vaccine, a study on the association between different hepatitis B virus strains and risk of developing liver cancer, or a review on “Cancer Vaccines: a new frontier in prevention and treatment,”
Biology Bytes author Teisha Rowland is a science writer, blogger at All Things Stem Cell, and graduate student in molecular, cellular, and developmental biology at UCSB, where she studies stem cells. Send any ideas for future columns to her at science@independent.com.



