County Psych Facility Needs More Beds
Plans for Additional Treatment Space Mean Hope for the Mentally Ill

If Deedrea Edgar can’t work the county’s mental health system, then chances are no one can. For the past seven years, she has been the go-to attorney in the Public Defender’s office for cases involving mental-health issues. Before that, Edgar worked as the patient advocate for the county’s Department of Alcohol, Drug, and Mental Health Services (ADMHS). If that weren’t enough, her father, Jack, was a defining presence within the Santa Barbara County Sheriff’s office, where, among other things, he assembled and trained the department’s first SWAT squad. And yet, when Deedrea Edgar tried to get county mental-health-crisis teams to help a relative in the throes of psychotic episodes, she might as well have called Ghost Busters.
In the past 12 years, Edgar has called for help six times, always in a crisis. Though law-enforcement officers have promptly shown up, it has been hit-and-miss with the mental-health-assessment team. For example, in September 2011, Edgar became concerned about her family member’s immediate safety and, to a lesser extent, about her own. Under the state’s well known 5150 law, individuals can be held against their will in psychiatric facilities if it’s determined they pose an imminent danger to themselves or others, or if they are deemed “gravely disabled,” which means they can’t feed, bathe, or clothe themselves. In Santa Barbara County, only county mental-health workers can make that evaluation. The sheriff deputies arrived, but in a phone conversation with the assessment-team leader, Edgar was unable to persuade Mental Health to take action. Her only remaining option was to press charges against her own family member, in the throes of a mental-health crisis. She felt she had no choice. “I didn’t want to be going to any funeral,” she recounted. “And that seemed like a likely alternative at the time.” Her relative was supposed to be psychologically assessed at county jail. If that happened, Edgar doesn’t know. She does know, however, that he was released into the general inmate population, where he got punched out by the reigning alpha inmate, spent 30 days in protective isolation, and was charged with two felony counts for his threatening behaviors.
Edgar’s family member would eventually be released and the charges dropped. Then — about five months ago — there was another flare-up. In the process, Edgar’s relative accidentally cut himself, but didn’t realize he was even bleeding. Again, Edgar called law enforcement. Again, they contacted Mental Health. And again, the mental-health-crisis workers, Edgar said, declined to come, telling the deputies that he did not meet the 5150 criteria. Ultimately, Edgar’s relative was escorted to the Cottage Hospital Emergency Room, where Edgar and other family members spent hours tag-teaming him into the next morning to ensure he didn’t leave. Eventually, Edgar managed to get him placed in a hospital outside the county, where he’s still residing after five months. “Would you want your grandmother suffering from Alzheimer’s booked into county jail because there was no other place to go?” Edgar demanded. “But we do it all the time with the mentally ill.”
For the record, regional mental-health administrator Andrew Vesper said he’s precluded by confidentiality laws from discussing the details of specific cases. He stressed that crisis workers do not simply refuse to respond unless they’ve “triaged the situation” with the first responders and any family members involved. And most emphatically, he denied that the availability of acute-care beds for 5150 patients — or the county’s infamous lack thereof — influences the decisions made by the county’s crisis-response team. “I would take serious offense,” he said, “at anyone saying we refused to respond to a crisis because of lack of beds.”

Making Room at the Inn
There are a host of complicated problems confounding the thousands of family members such as Edgar who scramble to secure care for their seriously mentally ill relatives in Santa Barbara County. But one of the most persistent is the acute shortage of bed space available. For the last 30 years, Santa Barbara County’s Psychiatric Health Facility (PHF) has only 16 acute-care beds. That unit — colloquially referred to as “the Puff Unit” — is located near the county jail on Camino del Remedio Road. The county also contracts for five additional acute-care beds at two mental-health facilities in Ventura County.
The Puff Unit is designed to function as a psychiatric intensive-care ward, holding the most severe cases until their condition can be stabilized. For nearly 30 years, elected officials, psychiatric professionals, law-enforcement leaders, and a host of patient advocates have complained about the lack of beds. Grand juries have repeatedly weighed in, urgently demanding corrective action be taken.
In that time, nothing has been done.
And nothing, it seemed, could be done. Ever. Until now.
For the first time in eons, a constellation of circumstances — some the product of national political forces, others the result of local dynamics — have conspired to create genuine opportunity to significantly change how mental-health services are provided in Santa Barbara County.
Immediate help seems to be coming first from Santa Maria in the form of Chuck Cova — the über-executive guiding the ship of Marian Regional Medical Center, a large hospital facility serving North County. While most hospitals across the country are retreating from mental-health services as too expensive to operate, Cova is talking about opening a new acute-care wing with 20 beds for 5150 patients and another 15 beds for geriatric psychiatric patients. The project, a joint partnership with the County of Santa Barbara and Telecare, a private mental-care provider, will be housed on the site of the now defunct Valley Community Hospital located in Santa Maria. Cova has been described by admirers as “a human wrecking ball” when it comes to overcoming obstacles. Given the scope and complexity of his undertaking, he’ll no doubt need to be. Even if Cova succeeds, however, it would be several years before the new facility could open.
At the same time, on the South Coast, a confederation of patient activists spearheaded by Families ACT! — a group led mostly by mothers who have lost adult children to the revolving door of mental illness, drug abuse, incarceration, overdose, and suicide — has unveiled an equally ambitious effort to create a continuum-of-care campus somewhere on the South Coast, envisioned as a mix of 60 affordable rental units with another 60 beds of residential crisis care that’s now nonexistent on the South Coast. While these facilities would not include any PHF beds, per se, they would include a range of structured residential care to help those beset by the twin afflictions of mental illness and substance abuse. As envisioned, this would provide patients getting out of the Puff much needed “step-down” care. It would also provide patients who relapse a range of fall-back options short of eviction and the streets. As planned, the mental-health services would be funded with revenues generated by the rental units to minimize the customary reliance upon grants. If built, that would be a first in Santa Barbara. These plans — barely off the drawing board — are undeniably audacious but have attracted the sustained attention of governmental and health-care heavy hitters.
And lastly, there’s the Affordable Care Act, otherwise known as Obamacare. Starting next January, about 25,000 low-income adults throughout Santa Barbara County — who earn less than $14,000 a year — will be eligible to apply for and receive MediCal coverage. Of those, about 500 are now uninsured county mental-health clients for whom the county can claim no compensation or remuneration. The Affordable Care Act not only expands the number of individuals eligible for coverage but also expands the extent of the compensation. Under most circumstances, the county can only be reimbursed for 50 percent of costs under existing MediCal formulas. Under Obamacare, the federal government will provide 100 percent compensation for new enrollees for the first three years, and 90 percent after that. How big of a gap in treatment the new coverage bridges remains unknown, but it’s clear that the strain on ADMHS, perhaps the most fiscally beleaguered of all county departments, will be considerably less.

The Tipping Point
None of these new opportunities emerged overnight. But the stress generated by the chronic shortage of beds clearly brought the county’s long-simmering mental-health-care crisis to a boil. Tragically igniting the torch was Clifford Detty, a 46-year-old diagnosed with paranoid schizophrenia. On the night of April 28, 2010, he was transported from Santa Maria’s Marian Regional Medical Center to the county’s PHF. Detty, who as a young man was an accomplished athlete, suffered from mental-health and substance-abuse issues. While his boyhood pal Robin Ventura went on to play major-league baseball, Detty spent his last night on earth under the influence of methamphetamine, arms and legs strapped to a gurney, agitated, combative, thrashing about, unable to follow instructions, hearing voices, screaming, and yanking at his straps. At PHF, Detty was further restrained, put in seclusion, and given antipsychotic medications.
By 5:30 the next morning, he was dead.

His father, Richard Detty — a retired owner of a Santa Maria insurance brokerage — has sued PHF in federal court, claiming his son was given too many antipsychotic medications in too short a time. In addition, he claimed PHF personnel failed to follow their own seclusion and restraint protocols. Had they taken his son’s vital signs every 15 minutes — as required — Detty claims his son would still be alive today. Instead, he charged, they checked only once. “His heart just quit,” his father said. “It burned out.”
The Detty case is not scheduled to go to trial until July 30, but its impact has already been felt. In January 2011, federal Medicare inspectors released a scathing 142-page report documenting a laundry list of problems: The Psychiatric Health Facility failed to report Detty’s death in a timely fashion, it consistently operated below minimal staffing levels, it failed to dispense opiates and other medications properly, patients were poorly discharged, and food was prepared in unsanitary conditions. By May, county officials had persuaded the federal inspectors they’d rectified the problems and were in full compliance. In August, however, the feds conducted an unannounced follow-up inspection. The inspectors found PHF personnel were too quick to put volatile patients in seclusion and restraints and did not follow their own protocol when doing so.
On October 12, 2011, the feds notified ADMHS director Ann Detrick that PHF’s shortcomings “substantially limit the hospital’s capacity to render adequate care to patients or are of such a character to adversely affect patient health and safety.” Accordingly, the feds notified Detrick they would be moving to terminate PHF’s Medicare contract as of January 2013. That would effectively shut the facility down.
The Slow Bleed
While the Psychiatric Health Facility was facing these problems, its overseeing department, ADMHS, had become the bureaucratic embodiment of post-traumatic stress disorder, lurching from one catastrophic emergency to the next. Back in 2007, the department had been put on notice that it had over-billed the state Department of Mental Health to the tune of $31 million — today, that number has been whittled down to $4.5 million — and would have to pay it back. Since then, the department has hacked funding for adult mentally-ill services by $14 million, and the number of employees staffing county mental-health clinics plunged from 185 to 100. At the same time, however, the county was forced to increase funding for the Puff Unit by $2 million, most of which was going to the increased number of mentally ill indigents in need of immediate care.

Making matters worse — at least for mental-health patients and their families — were events taking place outside the challenged orbit of ADMHS. Cottage Hospital, which had long accepted involuntary 5150 patients, stopped doing so in 2002; they proved too challenging, too time consuming, too legally demanding, and too costly. Then in 2004, St. Francis Hospital, now defunct, shut down its geriatric psychiatric unit. St. John’s Hospital in Oxnard briefly took up the slack, but it, too, soon went out of business. In 2007, Cottage terminated its contract with ADMHS and stopped accepting county mental-health clients altogether. That’s because county mental-health officials had abruptly announced that Cottage’s reimbursement rates would be cut by 40 percent. And in March 2009, the Salvation Army pulled the plug on an 86-bed drug- and alcohol-rehabilitation facility in Carpinteria that had offered poor and indigent addicts a much-needed residential treatment program.
The federal threat to shut down the PHF Unit in 2011 proved the last straw. The number of patients placed in seclusion and restraints dropped by half, and Ann Detrick, the beleaguered head of a beleaguered department, was summarily “resigned” as director of ADMHS. County supervisors announced with great fanfare that the status quo was no longer acceptable, and two major audits were ordered — at a cost of $265,000 — of the county’s inpatient and outpatient mental-health services. The results of those investigations will be made public before the Board of Supervisors in May. People who’ve received sneak previews by the consultants say the results are “scathing.”

Red Alert
In keeping with the new-broom policy, last December, the county hired a new medical director, Dr. Leslie Lundt, to run the Psychiatric Health Facility. An expert in the psycho-pharmacological needs of the severely bipolar, Lundt spent the last two years working at the Puff Unit at Ventura County’s Hillmont House, where she established the sort of step-down crisis residential treatment facility the South Coast is sorely lacking. Lundt stated Santa Barbara has less than half the PHF beds it needs for a county of 400,000, the bare minimum being 40. But since the county Puff facility is a stand-alone building — and not part of a hospital operation — the unit is restricted to 16 beds despite the fact that it was built to hold 25. This restriction has been in effect since the early 1980s, when the county’s public hospital closed. Santa Barbara is hardly unique in its paucity of PHF beds. But even so, it compares poorly with Ventura County, which offers more than twice as many acute-care beds per capita. In fact, if Santa Barbara were merely to meet the statewide average of 17 beds per 100,000, it would have around 70.
When the Santa Barbara PHF is full, Lundt said, everything else “backs up.” Emergency rooms and the county jail feel the pinch most immediately. And PHF is forced to juggle patient populations that aren’t easily juggled. About 25-33 percent of her case load are geriatric psychiatric patients. A small group comes from the county jail. And nearly half of her patients are homeless. All have different needs; all pose different risks. “We have little old ladies at PHF,” she said. “And we have young guys from the county jail.”
Currently, about 400-500 patients are sent to PHF each year on involuntary 5150 holds. About 11 percent are known as “frequent flyers,” meaning they’ve been held before within a 30-day period. On the South Coast, mental-health-crisis teams respond to about 100 calls for 5150 evaluations a month. Of those, 45 percent are determined to be 5150-worthy. Not all are eligible for the PHF. For example, the PHF does not accept minors. Nor does it accept individuals on drugs or alcohol. It is not medically licensed — or equipped — to deal with people going through drug withdrawal at the same time they experience a psychotic break. That’s a big problem because so many individuals experiencing an acute mental-health crisis have addiction issues.
In each of the past five years, anywhere from 220 to 446 patients have been sent to Ventura facilities. To treat the patient, Lundt stressed, the whole family must be involved. That’s significantly harder to do when families have to travel long distances. It’s also much more expensive for the county — which spends $1.3 million a year securing out-of-county care for its 5150 population — to send patients elsewhere. MediCal will reimburse the county 50 percent for its cost of PHF patients; it reimburses nothing for patients sent out of county.
Santa Barbara County is now seeking to rectify its shortage — at least in the short-term — by securing two additional PHF beds from the Ventura County contractors. But Lundt cautioned that there are not enough beds on the South Coast. “Last week, the San Luis [Obispo] PHF was full. We were full. The two Ventura facilities were full,” she said. “So where do these people go? This has happened a couple times since I’ve been here, and I’ve only been here a few months.”

Jail Time
The county jail has long been Santa Barbara’s largest holding facility for the mentally ill. Of that there can be no dispute. How the shortage of Puff beds has affected it, however, is much harder to document. The new commander, Laz Salinas, said the jail does not track how many inmates have been evaluated or how many have been transferred to PHF. The jail does maintain four protective-isolation holding cells that can be made available for inmates in psychological distress, as well as two step-down cells. In the past five to six weeks, he said, all four cells have been occupied at the same time only once. Salinas noted that 14-16 percent of all jail inmates in one recent week were under psychiatric care or receiving medications.
Several years ago, the jail hired a private contractor, Corizon, to help inmates with mental-health issues. Medications continue to be prescribed by the jail psychiatrist, but Corizon employs two licensed social workers, one marriage and family therapist, and one psychiatric RN, though not all are on call at the same time. The contractor is now renegotiating with the county jail, reportedly asking for a 3.6 percent increase, and is also seeking to service the county’s juvenile facilities.
The decision to privatize psychiatric medical services at the jail has, from the beginning, been controversial.
Suzanne Riordan with Families ACT! frequently denounces the quality of Corizon’s care. Too often, she claims, patients have gone without medications or have been incorrectly medicated. And, she argues, people with addiction and mental-health issues should never be put in jail in the first place. “These are not criminals,” said Riordan. “These are fragile human beings who get into self-medicating.” Riordan became politically active after her 23-year-old son — who’d struggled with addiction, mental-health issues, and incarceration since age 15 — died of an overdose in 2005.
For Riordan, the big issue has been the system’s chronic inability to address, let alone resolve, issues afflicting patients dealing simultaneously with both mental illness and substance abuse. Treatment is not just more humane; she cited county studies indicating it’s cheaper by roughly 30-40 percent. To that end, Riordan has teamed up with affordable-housing developer guru Frank Thompson — a savvy deal maker with expertise in tax-credit financing — and Phoenix House, one of the few private mental-health operators providing affordable treatment for the dually diagnosed. The team and its plan to create an integrated treatment campus with short-term and longer-term residential crisis care — 30-day, 90-day, and perhaps even longer — for the dually diagnosed with a job-training center in the culinary arts is undeniably impressive. The group has held six stakeholder meetings thus far, and the list of attendees is a who’s who of serious players, including Cottage Health System. But the big question remains, who will provide the land and where? Riordan said she’s hoping a government agency or nonprofit will supply the land; otherwise, the cost of the project will increase substantially.
Finding a Cure
Both major hospitals in the county, Cottage and Marian, have definitely felt the increased need for more 5150 facilities. In the past 14 months, Cottage Hospital reported processing 576 such patients in its emergency room — 41 a month — meaning they were medically evaluated and cleared. These tend to be high-maintenance patients for whom the intense stimulation of the emergency room can be too much. Making the situation even more volatile are the substances abused by many mentally ill. Stimulants such as “bath salts” and “spice” — increasingly popular drugs — can induce psychosis or prolong psychological agitation and take weeks to clear the body. For a while, Cottage had as many as 10 candidates for 5150 taking up space in its emergency rooms, some for as long as 96 hours. Cottage responded to the crunch by opening new “quiet treatment” areas — with dedicated staff — away from the hubbub of the emergency room, but only when three or more 5150 patients show up at the same time.
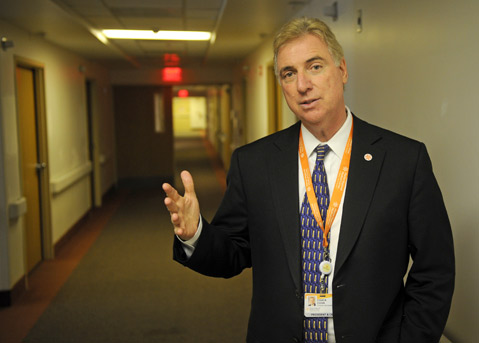
No one pretends that new PHF beds alone will solve the problem of a mental-health system that’s chronically underfunded, disjointed, and excruciatingly difficult for those most in need to access. But any “solution” that doesn’t include new beds is at best dubious. To that end, Chuck Cova of Marian Regional Medical Center— in Santa Maria — is boldly defying industry trends by pushing ahead with his plans for a new behavioral-health campus at the site of the old Valley Community Hospital. Cova explained that Marian could use its hospital license to provide as many as 20 PHF beds, sorely lacking to North County residents. Likewise, he’s proposed building a 14- to 18-bed geriatric psych facility, now found in only three California counties. He’s hoping to have financial projections ready by June. Cova — who recently spearheaded the construction of a brand-new hospital facility in Santa Maria— said permutations of this project had been in Marian’s strategic plans for the past six years. With the completion of the new hospital last year, he said, it freed up the old hospital structure. Cova said he confers regularly with Telecare and high-ranking county administrators such as Terri Maus-Nisich. The mere fact such talks are occurring, Nisich said, is “tremendous,” and “really exciting.” Cova believes the need is obvious. “We have a vision. We know the path we need to take to achieve that vision, and we know what road crossing we will encounter as we go down that path,” he said. “We’re going to take it one step at a time and see where it takes us. And we’re not going to stop unless someone turns the lights out on us.”



